Reviewer: S. Randhawa, M.D., Allergist/Immunologist and Assistant Professor at LSU (Shreveport) Department of Allergy and Immunology
A 58-year-old male with asthma and allergic rhinitis is seen for a follow-up at the allergy clinic. He only uses Albuterol PRN when he has wheezing in the course of upper respiratory tract infections. He was recently treated for acute pharyngitis and bronchitis with a 10-day course of Augmentin but still complains of nasal congestion. There is no nasal discharge, fever, chills or productive cough.
Past medical history (PMH)
Diabetes type 2 (DM2), allergic rhinitis, mild asthma, severe arthritis of the hands, right hand weakness secondary to remote stroke.
Medications
Nasacort (triamcinolone), Albuterol MDI, glyburide, rosiglitazone.
Physical examination
VSS.
HEENT: Pale boggy turbinates with 75% obstruction of the nasal cavity.
Chest: CTA (B).
CVS: Clear S1S2.
Abdomen: Soft, NT, ND, +BS.
Extremities: severe arthritis of both hands, and a R hand weakness secondary to remote stroke.

A hand with arthritic changes. Image source: Cicadas, a Creative Commons license.
Laboratory results
A CXR done by the PCP 5 days ago was negative.
What is the next step in the management?
The technique of use of the nasal spray and Albuterol inhaler was reviewed. Due to his arthritis and past stroke, the patient had a significant difficulty in using the devices correctly. He found it very difficult to push the activation parts of both theNasocort spray and the Albuterol inhaler. He was not able to point the nasal spray towards the ipsilatereal ear.
What would you recommend for this patient?
The Nasacort (R) spray was replaced with a Veramyst (R) spray which is activated by a squeezing button on the side of the device.
His Albuterol MDI was fitted with a VentEase (R) assist device and an AeroChamber (R).
Alternative options include:
- regular MDI with a large volume spacer and using the tidal breathing technique. No coordination between the activation of the MDI ("push") and breathing is required with this method because the patient takes regular breaths (tidal breathing)
- Diskus device - Flovent (fluticasone) or Advair (fluticasone/salmeterol)
The patient found the new devices much easier to use.
Final diagnosis
Medication noncompliance secondary to difficulty in using the asthma and allergic rhinitis treatment devices due to a neuromuscular impairment.
What did we learn from this case?
Asthma is the most common chronic respiratory disease, affecting up to 10% of adults and 30% of children (JACI, 2011).
Assist devices should be considered in patients with severe arthritis, stroke or other neuromuscular impairment who need to use asthma inhalers or nasal sprays. The standard devices and technique may not be sufficient in those patients, and therefore, may lead to poor treatment results.
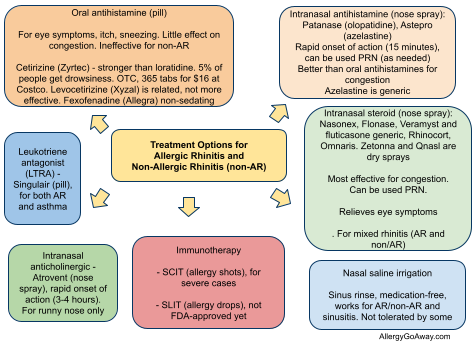
Treatment Options for Allergic Rhinitis (click to enlarge the image).
References
Aerosol Delivery Devices for the Geriatric Population. Helen M. Sorenson, MA, RRT, CPFT, American Association for Respiratory Care (PDF).
Modification of the spacer device. Use in the patient with arthritis or an artificial airway. Chest, Vol 102, 1243-1244, 1992.
Using an AeroChamber With Inhaled Medication. National Jewish Health.
Inhaler Technique Videos. Asthma Foundation http://goo.gl/5H5i
Published: 08/12/2008
Updated: 01/25/2011
Treatment Options for Allergic Rhinitis (click to enlarge the image).
References
Aerosol Delivery Devices for the Geriatric Population. Helen M. Sorenson, MA, RRT, CPFT, American Association for Respiratory Care (PDF).
Modification of the spacer device. Use in the patient with arthritis or an artificial airway. Chest, Vol 102, 1243-1244, 1992.
Using an AeroChamber With Inhaled Medication. National Jewish Health.
Inhaler Technique Videos. Asthma Foundation http://goo.gl/5H5i
Medications reference chart. Asthma Foundation http://goo.gl/ourq
Proper techniques for the administration of inhaled medications to treat asthma - AAAAI - Ask the Expert, 2011.
Published: 08/12/2008
Updated: 01/25/2011
No comments:
Post a Comment