Reviewer: S. Randhawa, M.D., Allergist/Immunologist, Fort Lauderdale, FL
Definition
Vocal cord dysfunction (VCD) is an upper airway obstruction caused by paradoxical closure (adduction) of the vocal cords on inspiration. VCD has also been misleadingly referred to as Munchausen stridor, episodic laryngeal dyskinesia, psychosomatic stridor, and emotional laryngeal asthma. VCD is more accurately described as paradoxical vocal fold motion.
Vocal cord dysfunction (VCD) is the paradoxical adduction of vocal cords during inspiration - normally, the vocal cords should abduct, or open during inspiration. VCD is often called an “asthma imitator” as these patients are often labeled as having a treatment-resistant asthma.
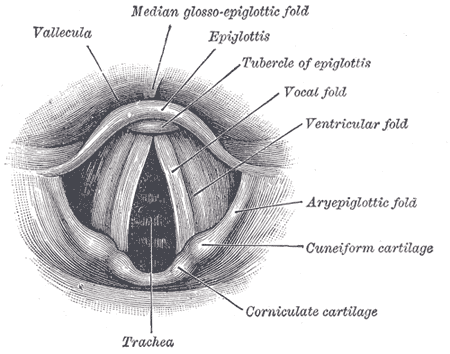
Laryngoscopic view of normal vocal folds. Image source: Wikipedia, Gray's Anatomy, public domain.
Etiology
The exact cause and pathogenesis of vocal cord dysfunction (VCD) remain unclear. Laryngeal hyperresponsiveness likely plays a role in a subset of patients. The origin and pathogenesis of VCD need to be better defined.
Symptoms of VCD
Vocal cord dysfunction (VCD) symptoms include:
- difficulty in breathing-in” - dyspnea on inspiration
- “fighting for breath”
- Wheezing, often inspiratory
- Stridor - inspiratory by definition
- Hoarse voice
- Dysphonia
- Chest or throat tightness
- Cough
Patients have described choking or stridor, and the stridorous sounds are loudest above the throat.
The typical patients with VCD is:
- Young female "overachiever" and/or athlete
- Middle-aged woman with some psychiatric history (anxiety or deppression) or occupation in health care
Diagnosis of VCD
Physical examination in VCD often shows inspiratory wheezing over larynx. Bronchodilators can paradoxically worsen the wheezing.
Spirometry not very helpful
Some findings on spirometry are often interpreted to suggest VCD, but recent studies have had varying results on how useful these are in the diagnosis of VCD. Spirometry may show reduced FEV1 and FVC with a preserved ratio and "blunted" inspiratory loop.
Rhinolaryngoscopy
The diagnosis is made with fiberoptic laryngoscopy while patient is symptomatic.
Diagnosis is made by direct visualization of the adduction of the vocal cords via rhinolaryngoscopy. However, the method used to provoke symptoms and adduction varies.
The standard for diagnosing VCD is to see adduction of the vocal cords during inspiration while the patient is having symptoms. This is done by flexible fiberoptic rhinolaryngoscopy. Seeing complete adduction of the vocal cords on inspiration with the formation of a small, posterior, diamond-shaped glottic chink is pathognomonic but seen in only 6% of cases.
Laryngoscopic evidence of VCD is found in 60% of patients during quiet respiration.
If vocal cords appear normal during laryngoscopy, several methods have been used to provoke symptoms:
- methacholine or histamine
- exercise
- breathing maneuvers (pant, breathe deeply, phonate, cough, sniffling)
Treatment of VCD
The early recognition and treatment of VCD are imperative to prevent the misdiagnosis and mismanagement of asthma. In addition, and confusingly, VCD and asthma can occur together.
Breathing exercises
Treatment ov VCD includes breathing exercises (pursed-lip breathing). Relaxation techniques, such as pursing lips, panting, and relaxing shoulders, should be implemented (see a list of VCD exercises from Medscape).
Speech therapy
Long-term therapy includes speech and behavioral treatment. In one study of adolescent female athletes, 95% were able to control their symptoms up to 6 months after speech therapy.
Other treatment options
Intermittent positive pressure ventilation (IPPV) may provide short term relief. Botulinum (Botox (R) injections the vocal cords have also been tried. Topical lidocaine spray is another option (aspiration due to decreased sensation may occur).
An anticholinergic inhaler was shown to be effective in some patients.
Long-term treatment of comorbid conditions (eg, proton pump inhibitors for GERD and laryngopharyngeal reflux) is also important.
References
Vocal cord dysfunction: an update. Leslie M. Gimenez, MD, Heidi Zafra, MD. Annals of Allergy, Asthma and Immunology, Volume 106, Issue 4, Pages 267-274 (April 2011).
VCD exercises. Medscape, 2011.
Use of videography in the diagnosis of exercise-induced vocal cord dysfunction: A case report with video clips. JACI, Volume 119, Issue 6, Pages 1329-1331 (June 2007)
Related reading
Olympic athlete hopeful improves her symptoms - and running time - after vocal training for vocal cord dysfunction. Daily Mail, 2011.
Video: Expiratory Vocal Cord Dysfunction and Laryngopharyngeal Reflux. CityAllergy: 62 yr old woman w/spasmodic coughing, wheezing and chronic dyspnea. Her PFTs showed a barely obstructive contour and she did not improve with inhaled or oral steroids. Her endoscopy showed evidence of LPR and posterior kinking of the larynx with expiration (classic VCD has inspiratory kinking).
Differential diagnosis of cough, a simple mnemonic is GREAT BAD CAT TOM. Click here to enlarge the image: (GERD (reflux), Laryngopharyngeal Reflux (LPR), Rhinitis (both allergic and non-allergic) with post-nasal drip (upper airway cough syndrome), Embolism, e.g. PE in adults, Asthma, TB (tuberculosis), Bronchitis, pneumonia, pertussis, Aspiration, e.g foreign body in children, Drugs, e.g. ACE inhibitor, CF in children, Cardiogenic, e.g. mitral stenosis in adults, Achalasia in adults, Thyroid enlargement, e.g. goiter, "Thoughts" (psychogenic), Other causes, Malignancy, e.g. lung cancer in adults).
Daniel E. Martin, PhD, SLP is the Director of the University of Chicago Voice Center, he specializes in VCD.
Vocal cord dysfunction (VCD) - paradoxical closure of vocal cords during inspiration - is a common mimicker of asthma. Immunology and Allergy Clinics of North America
Volume 33, Issue 1 , Pages 1-22, February 2013.
Vocal Cord Dysfunction: A Frequently Forgotten Entity - Case Rep Pulmonol. 2012 http://1.usa.gov/16dj2mI
Published: 05/09/2010
Updated: 03/09/2013
No comments:
Post a Comment