Reviewer: S. Randhawa, M.D., Allergist/Immunologist and Assistant Professor at NSU
A 39-year-old Caucasian female with a diagnosis of allergic rhinitis and asthma for 20 years is referred for evaluation to the allergy clinic. She was on Advair 250/50 bid (fluticasone/salmeterol) for two years, approximately four years ago, and then Advair was stopped by by her pulmonologist because her pulmonary function tests were normal. She is here for evaluation of allergic rhinitis by skin prick testing. She has increased shortness of breath with exercise. She reports loss of voice, cough, and shortness of breath when eating or laughing. The symptoms occur throughout the year. She also reports nasal congestion and for that, she takes Allegra D QAM and Allegra QPM . She rates the nasal symptoms as 5 out of 10 on a zero to 10 scale, when she is off the medication, and down to 1 to 2 out of 10 when she takes Allegra D. She also reports dry cough for 20 years which does not respond to albuterol. She exercises daily and uses albuterol 30 to 60 minutes before exercise, and then during her exercise routine for cough, change in her voice and shortness of breath. Thealbuterol helps, but it does not relieve her symptoms completely. She was on intranasal steroids in the past, but the spray was used inconsistently and she does not recall the effect of this treatment.
Past medical history (PMH)
Asthma, allergic rhinitis.
Medications
Allegra D in the morning and regular Allegra in the evening. Albuterol prn.
Social history
Positive exposure to tobacco smoke as a child, but none recently. Pets: She has two dogs. Occupation: physical therapist.
Family history
Mother with allergic rhinitis, daughter with exercise-induced asthma-like symptoms.
Physical examination
Vital signs stable.
Skin: No rashes. Eyes: Normal. Ears: Normal. Nose: Pale, boggy mucosa with clear discharge. Throat: Cobblestoning with posterior nasal drip. Respiratory system: Clear to auscultation bilaterally, no wheezing, rhonchi or crackles. Cardiovascular system: Clear S1, S2. Abdomen: Soft, non-tender, non-distended. Extremities: No edema.
Laboratory results
The patient had a spirometry, which showed FVC of 100%, FEV1 of 93%, FEV1/FVC ratio 0.74. We performed bronchodilator test, which was negative. Her FVC improved by 2%, FEV by 4% and she did not feel an improvement in her cough. She also had skin prick testing with aeroallergens and they were all negative.
What is the most likely cause of the patient's symptoms?
Vocal cord dysfunction.
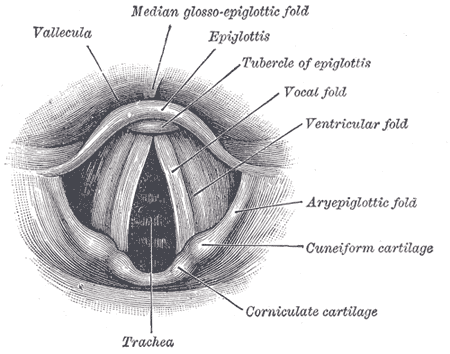
Laryngoscopic view of normal vocal folds. Image source: Wikipedia, Gray's Anatomy, public domain.
What treatment would you suggest?
This is a patient with long-standing history of shortness of breath, dyspnea on exertion, cough, change in her voice and postnasal drip. Currently, there is no convincing evidence of asthma, although she has exercise-induced symptoms. Vocal cord dysfunction (VCD) is strongly suspected and we would like the patient to followup with ENT for a rhinolaryngoscopic exam of her vocal cords to evaluate for vocal cord dysfunction. Rhinitis is most likely non-allergic. Skin prick testing is negative.
We advised the patient to stop Allegra and Allegra D and to use Veramyst two sprays daily. In order to be completely certain that asthma does not play a major role in her symptoms, she may need to have a methacholine challenge at her followup visit.
Final diagnosis
Vocal cord dysfunction (VCD).
Summary
Vocal cord dysfunction (VCD) is an an abnormal adduction of the vocal cords during the respiratory cycle (especially during the inspiratory phase) that produces airflow obstruction at the level of the larynx. Vocal cords should be open during inspiration. Paradoxically, they close during inspiration in patients with VCD.
VCD frequently mimics persistent asthma and is often treated with high-dose inhaled and/or systemic corticosteroids, bronchodilators, and may lead to multiple emergency department visits and hospitalizations.
Helpful hints to the diagnosis of VCD:
- patients reports symptoms in their throat or upper chest rather than in their chest, e.g. the typical chest tightness in asthma
- voice changes during the attack, e.g. hoarseness or loss of voice
- trouble "getting air in" (VCD) rather than getting air out (asthma)
- stridor (VCD) rather than wheezing (asthma)
- no relief with bronchodilator (albuterol) in VCD
References
Vocal Cord Dysfunction. Praveen Buddiga. eMedicine Specialties > Allergy and Immunology > Asthma.
Vocal Cord Dysfunction: Paradoxical Vocal Cord Motion - A Thorough Review. Grand Rounds Presentation, UTMB, Dept. of Otolaryngology. Todd M. Weiss, Francis B. Quinn, Jr., M.D.
Vocal cord dysfunction. Deckert J, Deckert L. Am Fam Physician. 2010 Jan 15;81(2):156-9.
Use of videography in the diagnosis of exercise-induced vocal cord dysfunction: A case report with video clips. JACI, Volume 119, Issue 6, Pages 1329-1331 (June 2007)
Related reading
Breathing disorder can be difficult to detect. USA Today, 2011.
Olympic athlete hopeful improves her symptoms - and running time - after vocal training for vocal cord dysfunction. Daily Mail, 2011.
Long-ago asthma diagnosis didn’t explain boy’s difficulty breathing - The Washington Post http://wapo.st/QGMfTC
Video: Expiratory Vocal Cord Dysfunction and Laryngopharyngeal Reflux. CityAllergy: 62 yr old woman w/spasmodic coughing, wheezing and chronic dyspnea. Her PFTs showed a barely obstructive contour and she did not improve with inhaled or oral steroids. Her endoscopy showed evidence of LPR and posterior kinking of the larynx with expiration (classic VCD has inspiratory kinking). Daniel E. Martin, PhD, SLP is the Director of the University of Chicago Voice Center, he specializes in VCD.
Published: 03/17/2009
Updated: 11/20/2012
5 comments:
What do you think of amitriptyline use?
http://www.dovepress.com/the-successful-treatment-of-vocal-cord-dysfunction-with-low-dose-amitr-peer-reviewed-article-JAA
Re: "What do you think of amitriptyline use?"
It's just one small study, isn't it? Too early to say. Works on the psychological component of the condition.
In psychogenic paradoxical cord movement is the use of a paralytic agent (intralaryngeal injection of botulinum toxin) effective?
Botulinum toxin injections are used for adductor spasmodic dysphonia. This condition is different from vocal cord dysfunction (VCD). Botulinum has been used for VCD too, but on a case by case basis. See the references below for more information:
Botulinum toxin injection and airflow stability in spasmodic dysphonia.
http://www.ncbi.nlm.nih.gov/pubmed/16500438
Injection for Spasmodic Dysphonia (video)
http://www.fauquierent.net/voicesd.htm
[Vocal cord dysfunction. An important differential diagnosis to bronchial asthma]
http://www.ncbi.nlm.nih.gov/pubmed/15007522
I had almost the exact same symptoms from age 14 and was forced to stop running at age 15. The condition stayed with me and by age 36 I had lost my ability to sing due to the gagging that would occur with any strain. Also experienced difficulties speaking when stressed and walking in cold weather.
Was diagnosed with vcd at age 38.
Respiratory physio-therapist showed me how to stretch the muscles of my jaw and told me to rinse my nose with saline twice daily and to gargle at least once a day (I use saline for that as well). Also to always chew strong lemon chewing gum during exercise, have a little lemon in my drinking water, (also always with me during exercise).
She gave me an interval training schedule. 15 min warmup, strain 1 min relax 6 min. Always breathe through my nose in the low stages of training and if possible during high intensity as well. Also she showed me how to get back to nose breathing after strain or if the condition was activated.
Chin towards chest inhale three short sniffs of air through my nose and repeat if needed.
This is all it took to improve my health. I can now exercise and sing again! I had this problem between ages 14 to 38 and now at age 39 my quality of life is better than ever before.
Was misdiagnosed with asthma, allergy to cats, and panic anxiety.
Post a Comment