Author: V. Dimov, M.D., Allergist/Immunologist and Assistant Professor at University of Chicago
Reviewer: S. Randhawa, M.D., Allergist/Immunologist and Assistant Professor at NSU
What are sinuses?
Sinuses are empty cavities within your cheek bones, around your eyes and behind your nose. You have 4 sinuses on each side of your head. There is a large sinus under your eye and another above your eye on each side. If you drop a line between your ears and another line down the center of your face, where those lines intersect is another sinus (sphenoid sinus). Then, connecting all three of these sinuses is what is called the ethmoid sinus, which is more of a labyrinth - like an egg-cartonlike group of sinuses.
What is sinusitis?
If your stuffy nose and cough last longer than 10 days, you may have more than a cold. Rhinosinusitis is a swelling of your nasal sinuses. It is often called sinusitis or a sinus infection.
How do I know if I have sinusitis?
You may experience any of the following:
- pressure around your nose, eyes or forehead
- stuffy nose
- thick, yellow or green drainage from your nose
- bad-tasting post-nasal drip
- cough
- head congestion, ear fullness or a headache
- toothache, tiredness and, occasionally, fever
Types and Causes of Sinusitis
Acute sinusitis refers to sinusitis symptoms that last less than 4 weeks. Most acute sinusitis starts as a regular cold from the common cold viruses and then becomes a bacterial infection.
Chronic sinusitis is when symptoms last 3 months or longer (more than 12 weeks). The cause of chronic sinusitis is a combination of swelling and infection. A CT scan can help to see if you have sinusitis or not.
Recurrent sinusitis occurs when 3 or more acute episodes happen in a year.
What are the risk factors for chronic sinusitis?
Allergic rhinitis
Allergic rhinitis puts you at risk for developing sinusitis because allergies can cause swelling of the nasal mucosa and blockage of the sinuses. This blockage prevents the sinuses from draining, and increases the risk of developing infection (bacterial sinusitis).
If your skin test is positive for allergies, your allergist can prescribe medications to control the swelling such as nose spray This can reduce your risk of developing an infection.
Immunodeficiency
Immune problems may decrease your ability to fight infections. Such problems include low levels of immunoglobulins (IgG, IgM, IgA), also called antibodies. Some patients have low level of antibodies to a common bacteria called Pneumococcus. This may lead to chronic or recurrent sinusitis.
A board-certified allergist can test quickly and reliably for both allergies and immunodeficiency.
Anatomical problems
Problems with the structure of your nose - such as narrow nasal or sinus passages, tumors or a shifted (deviated) nasal septum can also cause sinusitis. A CT scan can show such anatomocal problems. Surgery is sometimes needed to correct them.
Many patients with recurring or chronic sinusitis have more than one factor that puts them at risk of infection.
Diagnosis of sinusitis
To diagnose sinusitis, an allergist may order the following tests:
- allergy skin testing (blood testing is an alternative)
- antibody levels for IgG, IgM, IgA, and pneumococcal serotypes, complete blood count
- CT scan of the sinuses
Your physician may also perform an endoscopic examination. This involves inserting a narrow, flexible endoscope (a device with a light attached) into the nasal cavity through the nostrils after local anesthesia.
Treatment of sinusitis
Sinusitis requires a mix of treatments. You may need a medication to reduce nasal blockage and control allergies, which helps keep the sinus passages open such as steroid nasal spray.
If bacterial sinusitis is present, you will need an antibiotic.
For people with allergies, long-term treatment such as allergy shots can control allergic symptoms and prevent sinusitis.
Several non-drug treatments can also be helpful. These includes sinus rinses with distilled salty water.
Some patients may need surgery to correct the structure of your nose by an otorhinolaryngologist, or an ear-nose-throat physician (ENT).
References
Experts Discuss the Causes of Sinusitis. NYTimes, 2012.
Sinusitis. AAAAI.
Published: 02/28/2012
Updated: 03/18/2012
Showing posts with label Sinusitis. Show all posts
Showing posts with label Sinusitis. Show all posts
Saline Sinus Rinse/Flush - Patient Education Videos
Editor: V. Dimov, M.D., Allergist/Immunologist, Assistant Professor at University of Chicago
Saline nasal irrigation bathes the nasal cavity with liquid by instilling saline into 1 nostril and allowing it to drain out of the other nostril (typically, it drains from both nostrils and the mouth). Only use sterile, distilled, filtered water (using a filter with an absolute pore size of 1 μm or smaller), or previously boiled water for nasal irrigation.
NeilMed Sinus Rinse Video.
Pediatric Nasal Saline Flush/Rinse. Fauquier ENT | January 28, 2008 | This video shows a young child performing saline flushes to his nose without assistance. Indeed, kids older than 5 years are able to perform flushes without difficulty.
Adult Saline Sinus Rinse/Flush. Fauquier ENT | December 05, 2007 | Patient performing a saline flush to his nose. This procedure is often performed by patients who have chronic sinusitis or allergies.
Techniques and devices
Techniques and devices include:
- low positive pressure from a spray or squirt bottle
- gravity-based pressure using a neti pot or other vessel with a nasal spout
Indications
A range of conditions may respond to saline nasal irrigation but the evidence supporting its use is less conclusive:
- allergic rhinitis
- acute upper respiratory tract infections (URTI)
- rhinitis of pregnancy
- acute rhinosinusitis
The exact mechanism of action of saline nasal irrigation is unknown. Saline nasal irrigation may improve nasal mucosa function through direct cleansing; removal of inflammatory mediators, and improved mucociliary function, as suggested by increased ciliary beat frequency.
Adverse effects
Fewer than 10% of patients reported adverse effects:
- self-limited sensation of ear fullness
- "stinging" of the nasal mucosa
- rarely epistaxis
-infections. Louisiana Department of Health and Hospitals warned against improper use following the deaths of two people who were infected with Naegleria fowleri after using tap water to irrigate their sinuses. Read more here: Is Rinsing Your Sinuses Safe?
Contraindications
Contraindications for saline nasal irrigation include:
- incompletely healed facial trauma
- increased risk for aspiration, such as intention tremor or other neurologic or musculoskeletal problems.
Recommendations
- For chronic rhinosinusitis, nasal irrigation is an effective adjunctive therapy (level of evidence, A).
- Limited evidence for effective adjunctive treatment of irritant or allergic rhinitis, viral upper respiratory tract infection, and postoperative care after endoscopic sinus surgery (level of evidence, B).
- rhinitis of pregnancy, acute rhinosinusitis, sinonasal sarcoidosis, and Wegener's granulomatosis (level of evidence, C).
Mayo Clinic: What can you do about that runny nose and nasal congestion? Medications are one option, but so is nasal cleansing.
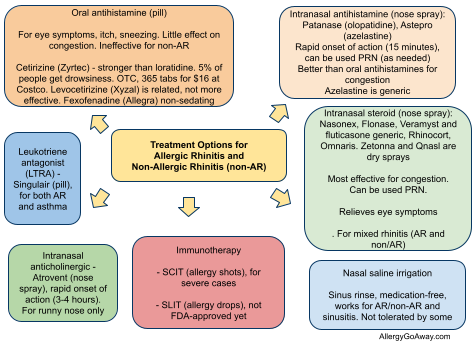
Treatment Options for Allergic Rhinitis (click to enlarge the image).
References
Use of Saline Nasal Irrigation Reviewed. Laurie Barclay, MD. Medscape, 2009.
Saline Nasal Irrigation for Upper Respiratory Conditions. Am Fam Physician. 2009 November 15; 80(10): 1117–1119 (PDF).
SinuSurf (nasal saline rinse with surfactant) associated with loss of smell "for months to years". Discontinue use (PDF) http://goo.gl/awQUP
Neti Pot, Nasal Irrigation - Pros and Cons and Slideshow. WebMD, 2011.
North Louisiana Woman Dies from Rare Ameba Infection. DHH warns residents about improper neti pot use, 2011.
Is Rinsing Your Sinuses Safe? FDA replies: http://goo.gl/XL5bJ
Chronic sinus infections with mycobacteria associated with sinus rinses with tap water (nasal washing) http://goo.gl/wiV12
Published: 02/07/2011
Updated: 08/27/2012
Saline nasal irrigation bathes the nasal cavity with liquid by instilling saline into 1 nostril and allowing it to drain out of the other nostril (typically, it drains from both nostrils and the mouth). Only use sterile, distilled, filtered water (using a filter with an absolute pore size of 1 μm or smaller), or previously boiled water for nasal irrigation.
NeilMed Sinus Rinse Video.
Pediatric Nasal Saline Flush/Rinse. Fauquier ENT | January 28, 2008 | This video shows a young child performing saline flushes to his nose without assistance. Indeed, kids older than 5 years are able to perform flushes without difficulty.
Adult Saline Sinus Rinse/Flush. Fauquier ENT | December 05, 2007 | Patient performing a saline flush to his nose. This procedure is often performed by patients who have chronic sinusitis or allergies.
Techniques and devices
Techniques and devices include:
- low positive pressure from a spray or squirt bottle
- gravity-based pressure using a neti pot or other vessel with a nasal spout
Indications
A range of conditions may respond to saline nasal irrigation but the evidence supporting its use is less conclusive:
- allergic rhinitis
- acute upper respiratory tract infections (URTI)
- rhinitis of pregnancy
- acute rhinosinusitis
The exact mechanism of action of saline nasal irrigation is unknown. Saline nasal irrigation may improve nasal mucosa function through direct cleansing; removal of inflammatory mediators, and improved mucociliary function, as suggested by increased ciliary beat frequency.
Adverse effects
Fewer than 10% of patients reported adverse effects:
- self-limited sensation of ear fullness
- "stinging" of the nasal mucosa
- rarely epistaxis
-infections. Louisiana Department of Health and Hospitals warned against improper use following the deaths of two people who were infected with Naegleria fowleri after using tap water to irrigate their sinuses. Read more here: Is Rinsing Your Sinuses Safe?
Contraindications
Contraindications for saline nasal irrigation include:
- incompletely healed facial trauma
- increased risk for aspiration, such as intention tremor or other neurologic or musculoskeletal problems.
Recommendations
- For chronic rhinosinusitis, nasal irrigation is an effective adjunctive therapy (level of evidence, A).
- Limited evidence for effective adjunctive treatment of irritant or allergic rhinitis, viral upper respiratory tract infection, and postoperative care after endoscopic sinus surgery (level of evidence, B).
- rhinitis of pregnancy, acute rhinosinusitis, sinonasal sarcoidosis, and Wegener's granulomatosis (level of evidence, C).
Mayo Clinic: What can you do about that runny nose and nasal congestion? Medications are one option, but so is nasal cleansing.
Treatment Options for Allergic Rhinitis (click to enlarge the image).
References
Use of Saline Nasal Irrigation Reviewed. Laurie Barclay, MD. Medscape, 2009.
Saline Nasal Irrigation for Upper Respiratory Conditions. Am Fam Physician. 2009 November 15; 80(10): 1117–1119 (PDF).
SinuSurf (nasal saline rinse with surfactant) associated with loss of smell "for months to years". Discontinue use (PDF) http://goo.gl/awQUP
Neti Pot, Nasal Irrigation - Pros and Cons and Slideshow. WebMD, 2011.
North Louisiana Woman Dies from Rare Ameba Infection. DHH warns residents about improper neti pot use, 2011.
Is Rinsing Your Sinuses Safe? FDA replies: http://goo.gl/XL5bJ
Chronic sinus infections with mycobacteria associated with sinus rinses with tap water (nasal washing) http://goo.gl/wiV12
Published: 02/07/2011
Updated: 08/27/2012
Allergic fungal sinusitis (AFS)
Author: V. Dimov, M.D., Allergist/Immunologist and Assistant Professor at University of Chicago
Reviewer: S. Randhawa, M.D., Allergist/Immunologist and Assistant Professor at LSU (Shreveport) Department of Allergy and Immunology
Allergic fungal sinusitis is a chronic hyperplastic sinusitis with eosinophilic inflammation. It is associated with fungal allergens. The pathologic features are similar to allergic bronchopulmonary aspergillosis (ABPA). 5%-10% of patients with chronic rhinosinusitis who require surgery have AFS.
Causative fungi include Bipolaris, Curvularia, Alternaria, Drechslera, Helminthosporium, Fusarium, and Aspergillus. The most common cause of AFS is Bipolaris.
Clinical features of AFS
The typical typical patient is a young adult with a history of allergic rhinitis/chronic sinusitis which is refractory to therapy. Nasal blockage becomes worse as nasal polyps enlarge. CT of sinuses shows extensive mucosal disease with complete sinus opacification. There may be blood eosinophilia and elevated serum IgE.
Diagnostic criteria for AFS:
1. chronic sinusitis of at least 6 months with CT or MRI findings
2. nasal polyps
3. typical allergic mucin found at sinus surgery, with absence of tissue invasion
4. fungus in allergic mucin - histopathology/culture
Allergic mucin is often described as "peanut butter".
Treatment of AFS
Treatment consists of of surgical debridement and oral steroids.
Oral corticosteroids are usually initiated before surgery and are for three to four weeks postoperatively.
Antifungal agents have not been shown to significantly modify clinical course.
AFS is a chronic condition that requires life-long therapy. AFS recurrence varies in the range of 10-90%.
AFS is a chronic condition that requires life-long therapy. AFS recurrence varies in the range of 10-90%.
Related reading
Atrophic Rhinosinusitis: Progress Toward Explanation of an Unsolved Medical Mystery. Medscape, 2011.
Published: 05/09/2010
Updated: 03/09/2011
Pediatric sinusitis
Author: V. Dimov, M.D., Allergist/Immunologist and Assistant Professor at University of Chicago
Reviewer: S. Randhawa, M.D., Allergist/Immunologist and Assistant Professor at NSU
Nasal physiology
Mucociliary clearance can be tested by placing saccharin on the inferior turbinate and timing the onset of sweet taste in the mouth. The normal range is 7-11 minutes.
There is normal asymmetry of nasal mucosa swelling, with one side of nose swollen as a result of dilatation of veins in the inferior turbinate and the other side "open" - 80% of the population exhibits a nasal cycle, with reciprocal changes in airflow over 1-2 hours.
Anatomy of paranasal sinuses
Sinus is a Latin word for “fold” or “pocket”. Paranasal sinuses have an embryogenic origin from the nasal passage and are an integral component of the airway. Drainage pathways of the sinuses are complex and can be blocked during inflammation. Ostia are the sinus openings in the nasal cavity. They are 2-6 mm wide.
Paranasal sinuses have an embryogenic origin from the nasal passage and are an integral component of the airway. Drainage pathways of the sinuses are complex and can be blocked during inflammation.
The outflow tract of the maxillary sinus is positioned high on medial wall, therefore intact mucociliary apparatus required to move mucus and debris from sinus into nose.
The ethmoid sinus consists of 3 to 15 air cells (on left and right sides), separated by thin bony partitions. Each air cell drains by tiny ostium into middle meatus and the ostia are easily obstructed during URI.
The frontal sinus develops from anterior ethmoid cell and achieves supraorbital position by 6 years of age. It is an uncommon site of infection in pediatrics.
The sinus ostia are the drainage routes for paranasal sinuses - because of their small diameter (1.0-2.5 mm), they are easily occluded by mucosal inflammation. This is is similar to the blockage of Eustachian tube that can lead to otitis media.
How large are the ostia of the sinuses?
The size of ostium of the maxillary sinus is 2.5 mm, the ostia of the other sinuses are smaller - in the range of 1 mm.
Location of the openings of the sinuses
- Inferior meatus - opening of nasolacrimal duct.
- Middle meatus - frontal, maxillary and anterior ethmoids
- Superior turbinate - posterior ethmoids and sphenoid sinuses
Mnemonic
Sinuses listen to the following radio channels: FM AM / PS SS
Frontal sinus, Maxillary sinus, and
Anterior ethmoids drain into Middle meatus
Posterior ethmoids and Sphenoid sinus drain into
Sphenoethmoidal recess above Superior turbinate
Sinusitis
Sinusitis of less than 4 weeks’ duration is considered acute. Chronic sinusitis persists for more than 4 weeks.
Recurrent sinusitis is defined as 4 or more episodes of sinusitis per year. Each episode lasting 7-10 days and no symptoms during intervening periods. Sinusitis is mostly preceded by rhinitis and is rarely found without rhinitis.
The 1997 Rhinosinusitis Task Force thus proposed the term Rhinosinusitis instead of Sinusitis (reiterated in 2007 guidelines).
Diagnosis
The diagnosis is clinical most of the time.
Radiographic findings suggestive of acute sinusitis:
- diffuse opacification - most common finding in children with acute bacterial sinusitis
- mucosal swelling greater than 4 mm
- presence of air-fluid level - may not occur in children
Maxillary sinus aspiration recovered bacteria from 75% of children with abnormal radiographic findings (Wald et al, 1981).
History of persistent upper respiratory symptoms predicted abnormal findings on radiographs in 88% of children younger than 6 yr of age and in 70% of children older than 6 yr of age (Wald et al, 1986).
The frequency of bacterial sinusitis peaks by 6 years of age.
According to the current guidelines, the diagnosis of acute bacterial sinusitis does not require radiographic imaging in children younger than 6 yr of age with persistent upper respiratory symptoms. The diagnosis is based on clinical findings only. There is no consensus about the need for imaging for children older than 6 yr of age with persistent symptoms and for all children with severe or worsening symptoms.
Do you need an X-ray to diagnose sinusitis in children?
Acute sinusitis in children is likely if the symptoms persist for tnan 10 but less than 30 days and they are not improing. This predicts abnormal X-ray in 88% of children yonger than 6 years. They can be treated with an antibiotic withouth an X-ray.
The "story" is different in children older than 6 years - 30% of them had a normal X-ray and this group may not need an antibiotic. Only 75% of children with abnormal X-rays had a positive bacterial sinus aspirate.
Sinus Imaging for Diagnosis of CRS in Children - plain radiography has limited utility - CT and MRI have a major role (http://goo.gl/cNHHK).
Pathogens in pediatric sinusitis
From aspiration of maxillary sinus ((Wald et al, 1981):
- Streptococcus pneumoniae, 30% to 40%
- Haemophilus influenzae, 20%
- Moraxella catarrhalis, 20%
- Streptococcus pyogenes (group A streptococci), 4%
- no bacteria recovered from 25% of samples
The widespread use of pneumococcal vaccine has resulted in changes in prevalence. The recent data is from tympanocentesis studies of children with acute otitis media and showed decreased rate of infection with S pneumoniae and increased rate of infection with H influenzae. The data can be extrapolated to sinusitis - some ENTs consider the middle ear "a paranasal sinus."
Antibiotic resistance
- 35% of isolates of H influenzae and 100% of isolates of M catarrhalis are resistant to b-lactam antibiotics
- 25% to 50% of isolates of S pneumoniae resistant to penicillin (half are highly resistant)
"Plain old" amoxicillin will not help in those cases.
Treatment of Acute Sinusitis
References
Pediatric sinusitis. Ellen R. Wald, MD. Audio-Digest Pediatrics, Volume 55, Issue 14, July 21, 2009.
Acute and Chronic Rhinosinusitis: Practical Clinical Treatment Strategies. Nancy Otto, PharmD. Medscape, 11/2008.
Published: 05/29/2010
Updated: 03/30/2012
Reviewer: S. Randhawa, M.D., Allergist/Immunologist and Assistant Professor at NSU
Nasal physiology
Mucociliary clearance can be tested by placing saccharin on the inferior turbinate and timing the onset of sweet taste in the mouth. The normal range is 7-11 minutes.
There is normal asymmetry of nasal mucosa swelling, with one side of nose swollen as a result of dilatation of veins in the inferior turbinate and the other side "open" - 80% of the population exhibits a nasal cycle, with reciprocal changes in airflow over 1-2 hours.
Anatomy of paranasal sinuses
Sinus is a Latin word for “fold” or “pocket”. Paranasal sinuses have an embryogenic origin from the nasal passage and are an integral component of the airway. Drainage pathways of the sinuses are complex and can be blocked during inflammation. Ostia are the sinus openings in the nasal cavity. They are 2-6 mm wide.
Paranasal sinuses have an embryogenic origin from the nasal passage and are an integral component of the airway. Drainage pathways of the sinuses are complex and can be blocked during inflammation.
The outflow tract of the maxillary sinus is positioned high on medial wall, therefore intact mucociliary apparatus required to move mucus and debris from sinus into nose.
The ethmoid sinus consists of 3 to 15 air cells (on left and right sides), separated by thin bony partitions. Each air cell drains by tiny ostium into middle meatus and the ostia are easily obstructed during URI.
The frontal sinus develops from anterior ethmoid cell and achieves supraorbital position by 6 years of age. It is an uncommon site of infection in pediatrics.
The sinus ostia are the drainage routes for paranasal sinuses - because of their small diameter (1.0-2.5 mm), they are easily occluded by mucosal inflammation. This is is similar to the blockage of Eustachian tube that can lead to otitis media.
How large are the ostia of the sinuses?
The size of ostium of the maxillary sinus is 2.5 mm, the ostia of the other sinuses are smaller - in the range of 1 mm.
Location of the openings of the sinuses
- Inferior meatus - opening of nasolacrimal duct.
- Middle meatus - frontal, maxillary and anterior ethmoids
- Superior turbinate - posterior ethmoids and sphenoid sinuses
Mnemonic
Sinuses listen to the following radio channels: FM AM / PS SS
Frontal sinus, Maxillary sinus, and
Anterior ethmoids drain into Middle meatus
Posterior ethmoids and Sphenoid sinus drain into
Sphenoethmoidal recess above Superior turbinate
Sinusitis
Sinusitis of less than 4 weeks’ duration is considered acute. Chronic sinusitis persists for more than 4 weeks.
Recurrent sinusitis is defined as 4 or more episodes of sinusitis per year. Each episode lasting 7-10 days and no symptoms during intervening periods. Sinusitis is mostly preceded by rhinitis and is rarely found without rhinitis.
The 1997 Rhinosinusitis Task Force thus proposed the term Rhinosinusitis instead of Sinusitis (reiterated in 2007 guidelines).
Diagnosis
The diagnosis is clinical most of the time.
Radiographic findings suggestive of acute sinusitis:
- diffuse opacification - most common finding in children with acute bacterial sinusitis
- mucosal swelling greater than 4 mm
- presence of air-fluid level - may not occur in children
Maxillary sinus aspiration recovered bacteria from 75% of children with abnormal radiographic findings (Wald et al, 1981).
History of persistent upper respiratory symptoms predicted abnormal findings on radiographs in 88% of children younger than 6 yr of age and in 70% of children older than 6 yr of age (Wald et al, 1986).
The frequency of bacterial sinusitis peaks by 6 years of age.
According to the current guidelines, the diagnosis of acute bacterial sinusitis does not require radiographic imaging in children younger than 6 yr of age with persistent upper respiratory symptoms. The diagnosis is based on clinical findings only. There is no consensus about the need for imaging for children older than 6 yr of age with persistent symptoms and for all children with severe or worsening symptoms.
Do you need an X-ray to diagnose sinusitis in children?
Acute sinusitis in children is likely if the symptoms persist for tnan 10 but less than 30 days and they are not improing. This predicts abnormal X-ray in 88% of children yonger than 6 years. They can be treated with an antibiotic withouth an X-ray.
The "story" is different in children older than 6 years - 30% of them had a normal X-ray and this group may not need an antibiotic. Only 75% of children with abnormal X-rays had a positive bacterial sinus aspirate.
Sinus Imaging for Diagnosis of CRS in Children - plain radiography has limited utility - CT and MRI have a major role (http://goo.gl/cNHHK).
Pathogens in pediatric sinusitis
From aspiration of maxillary sinus ((Wald et al, 1981):
- Streptococcus pneumoniae, 30% to 40%
- Haemophilus influenzae, 20%
- Moraxella catarrhalis, 20%
- Streptococcus pyogenes (group A streptococci), 4%
- no bacteria recovered from 25% of samples
The widespread use of pneumococcal vaccine has resulted in changes in prevalence. The recent data is from tympanocentesis studies of children with acute otitis media and showed decreased rate of infection with S pneumoniae and increased rate of infection with H influenzae. The data can be extrapolated to sinusitis - some ENTs consider the middle ear "a paranasal sinus."
Antibiotic resistance
- 35% of isolates of H influenzae and 100% of isolates of M catarrhalis are resistant to b-lactam antibiotics
- 25% to 50% of isolates of S pneumoniae resistant to penicillin (half are highly resistant)
"Plain old" amoxicillin will not help in those cases.
Treatment of Acute Sinusitis
Recommendations form the current guidelines
For children with uncomplicated mild to moderate acute bacterial sinusitis without risk factors (age less than 2 yr; recent use of antibiotics; attendance at daycare), give amoxicillin or amoxicillin-clavulanate, 45 to 90 mg/kg per day (in 2 divided doses).
In acute sinusitis in children, you often have to use high dose amoxicillin (90 mg per kg) - 45 mg per kg is not helful because of resistance.
In penicillin allergy, you can use cefdinir, cefuroxime, or cefpodoxime for children with mild allergy; clarithromycin or azithromycin for children with type-1 hypersensitivity (but these have low activity against Haemophilus).
If there is no effect within 72 hr, consider increasing dose of amoxicillin-clavulanate to 80 to 90 mg/kg per day (2 divided doses).
Amoxicillin-clavulanate to 80 to 90 mg/kg per day should be used in:
- patients who do not improve within 72 hr
- those who have recently received antibiotics
- moderate to severe disease
These higher doses achieve concentration needed to eradicate most highly-resistant S. pneumoniae
How long should you treat with an antibiotic?
The minimum ciurse is 10 days. A simple rule is to treat until the patient becomes symptom free plus 7 more days.
When to change the antibiotic?
If children are treated with an antibiotic, they should start to get better within 48 hours, and should feel substantially better within 72 hours. If they do not feel better within 72 hours (3 days), you either got the wrong diagnosis or the wrong antibiotic. It is reasonable to start with amoxicillin/clavunate, and if there is no effect within 72 hours, switch to cefpodoxime.
What is the role of corticosteroids nose sprays?
Some studies show modest benefit of intranasal corticosteroids. Intranasal decongestants (eg, oxymetazoline form 3 days) or saline irrigation may be useful.
Pediatric sinusitis. Ellen R. Wald, MD. Audio-Digest Pediatrics, Volume 55, Issue 14, July 21, 2009.
Acute and Chronic Rhinosinusitis: Practical Clinical Treatment Strategies. Nancy Otto, PharmD. Medscape, 11/2008.
Sinusitis Practice Guideline Aims to Improve Diagnosis, Cut Antibiotic Use. AFP, 2007.
Antibiotic Treatment for Rhinosinusitis - Levofloxacin recommended for children with penicillin allergy? Medscape, 2012.
Related reading
FIT Corner Questions. Chapter 78 of the 6th edition of Middleton’s Allergy Principles and Practice, edited by N. Franklin Adkinson, et al. September 27, 2006. Chapter 78: Nasal Polyps and Sinusitis.
Antibiotic Treatment for Rhinosinusitis - Levofloxacin recommended for children with penicillin allergy? Medscape, 2012.
Related reading
FIT Corner Questions. Chapter 78 of the 6th edition of Middleton’s Allergy Principles and Practice, edited by N. Franklin Adkinson, et al. September 27, 2006. Chapter 78: Nasal Polyps and Sinusitis.
Humming increases airflow between the sinus and nasal cavities, which could protect against sinus infections. NYTimes, 2010.
Frequent otitis media during infancy linked to atopic dermaitis and asthma in later life. Medscape, 2010.
Unlike otitis media, visit rate for acute sinusitis among children did not decrease after pneumococcal conjugate vaccine, Pediatrics, 12/2010. http://goo.gl/gkwYm
The best price for azithromycin is at Costco: 18 tablets for $18.
SNOT-16 Assessment Tool for Acute Sinusitis takes 5 minutes - copyright protected by Washington University. Medscape, 2011.
Intranasal Treatment for Clogged Ears: ears are connected to the back of the nose via a tunnel called Eustachian tube. http://goo.gl/2XwD9
Mnemonics for sinusitis: PODS and C-PODS (end of PDF here)
SNOT-16 Assessment Tool for Acute Sinusitis takes 5 minutes - copyright protected by Washington University. Medscape, 2011.
Intranasal Treatment for Clogged Ears: ears are connected to the back of the nose via a tunnel called Eustachian tube. http://goo.gl/2XwD9
Mnemonics for sinusitis: PODS and C-PODS (end of PDF here)
Published: 05/29/2010
Updated: 03/30/2012
Adult Sinusitis: Brief Review
Author: V. Dimov, M.D., Allergist/Immunologist and Assistant Professor at University of Chicago
Reviewer: S. Randhawa, M.D., Allergist/Immunologist and Assistant Professor at NSU
Nasal physiology
Mucociliary clearance can be tested by placing saccharin on the inferior turbinate and timing the onset of sweet taste in the mouth. The normal range is 7-11 minutes.
There is normal asymmetry of nasal mucosa swelling, with one side of nose swollen as a result of dilatation of veins in the inferior turbinate and the other side "open" - 80% of the population exhibits a nasal cycle, with reciprocal changes in airflow over 1-2 hours.
Anatomy
Sinus is a Latin word for “fold” or “pocket”. Paranasal sinuses have an embryogenic origin from the nasal passage and are an integral component of the airway. Drainage pathways of the sinuses are complex and can be blocked during inflammation. Ostia are the sinus openings in the nasal cavity. They are 2-6 mm wide.
Sinusitis
Approximately 31-35 million Americans are affected by sinusitis every year (15% of the population).
Sinusitis of less than 4 weeks’ duration is considered acute. Chronic sinusitis persists for more than 4 weeks.
Recurrent sinusitis is defined as 4 or more episodes of sinusitis per year. Each episode lasting 7-10 days and no symptoms during intervening periods.
Acute Exacerbation of Chronic Sinusitis is the sudden worsening of chronic sinusitis that returns to baseline with treatment.
The term sinusitis is often interpreted as reflecting simply a bacterial sinus infection but the disease can have a significant allergic component.
Sinusitis is mostly preceded by rhinitis and is rarely found without rhinitis.
The 1997 Rhinosinusitis Task Force thus proposed the term Rhinosinusitis instead of Sinusitis (reiterated in 2007 guidelines).
Acute Sinusitis
Symptoms for up to 4 weeks. Viral most of the time. Bacterial in less than 5%. Patients with allergic rhinitis (AR) are more susceptible to acute sinusitis.
Duration of symptoms and definition
Less than 4 weeks - acute sinusitis
Reviewer: S. Randhawa, M.D., Allergist/Immunologist and Assistant Professor at NSU
Nasal physiology
Mucociliary clearance can be tested by placing saccharin on the inferior turbinate and timing the onset of sweet taste in the mouth. The normal range is 7-11 minutes.
There is normal asymmetry of nasal mucosa swelling, with one side of nose swollen as a result of dilatation of veins in the inferior turbinate and the other side "open" - 80% of the population exhibits a nasal cycle, with reciprocal changes in airflow over 1-2 hours.
Anatomy
Sinus is a Latin word for “fold” or “pocket”. Paranasal sinuses have an embryogenic origin from the nasal passage and are an integral component of the airway. Drainage pathways of the sinuses are complex and can be blocked during inflammation. Ostia are the sinus openings in the nasal cavity. They are 2-6 mm wide.
Location of the openings of the sinuses
- Inferior meatus - opening of nasolacrimal duct.
- Middle meatus - frontal, maxillary and anterior ethmoids
- Superior turbinate - posterior ethmoids and sphenoid sinuses
Mnemonic
Sinuses listen to the following radio channels: FM AM / PS SS
Frontal sinus, Maxillary sinus, and
Anterior ethmoids drain into Middle meatus
Posterior ethmoids and Sphenoid sinus drain into
Sphenoethmoidal recess above Superior turbinate
Sinusitis
Approximately 31-35 million Americans are affected by sinusitis every year (15% of the population).
Sinusitis of less than 4 weeks’ duration is considered acute. Chronic sinusitis persists for more than 4 weeks.
Recurrent sinusitis is defined as 4 or more episodes of sinusitis per year. Each episode lasting 7-10 days and no symptoms during intervening periods.
Acute Exacerbation of Chronic Sinusitis is the sudden worsening of chronic sinusitis that returns to baseline with treatment.
The term sinusitis is often interpreted as reflecting simply a bacterial sinus infection but the disease can have a significant allergic component.
Sinusitis is mostly preceded by rhinitis and is rarely found without rhinitis.
The 1997 Rhinosinusitis Task Force thus proposed the term Rhinosinusitis instead of Sinusitis (reiterated in 2007 guidelines).
Acute Sinusitis
Symptoms for up to 4 weeks. Viral most of the time. Bacterial in less than 5%. Patients with allergic rhinitis (AR) are more susceptible to acute sinusitis.
Duration of symptoms and definition
Less than 4 weeks - acute sinusitis
4-12 weeks - subacute sinusitis
Longer than 12 weeks - chronic sinusitis
Complications of acute sinusitis
Orbital cellulitis
Subperiostal, intraorbital or eyelid abscess
Cavernous sinus thrombosis
Meningitis
Subdural, epidural or brain abscesses
Osteomyelitis of frontal bone (Potts puffy tumor)
Chronic Sinusitis
Symptoms for more than 12 weeks. Not an "infection."
Eosinophilic Sinusitis
Allergic Fungal Sinusitis (click to read the article)
Complications of acute sinusitis
Orbital cellulitis
Subperiostal, intraorbital or eyelid abscess
Cavernous sinus thrombosis
Meningitis
Subdural, epidural or brain abscesses
Osteomyelitis of frontal bone (Potts puffy tumor)
Chronic Sinusitis
Symptoms for more than 12 weeks. Not an "infection."
Eosinophilic Sinusitis
Allergic Fungal Sinusitis (click to read the article)
Noneosinophilic Sinusitis
Noneosinophilic sinusitis is considered to have an infectious basis and is treated with antibiotics. Organisms found are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. If a patient has Pseudomonas aeruginosa or Staphylococcus aureus, cystic fibrosis should be considered in differential diagnosis.
Diagnosis
A limited CT of sinuses costs about the same as a standard plain film sinus series but is much more useful.
CT scan findings do not correlate well with symptoms.
Upper airway endoscopy can identify anatomic or mechanical disorders of the upper airway. Anterior rhinoscopy is an examination of the nasal cavity performed with a nasal speculum under good illumination. Usually done with a rigid rhinoscope.
The gold standard for diagnosis of bacterial sinusitis is sinus puncture and culture.
Treatment
Treatment of Acute Sinusitis
Over 70% of patients with acute rhinosinusitis improve after 7 days, with or without antimicrobial therapy.
NNT = 7: 7 patients must be treated to achieve one additional positive outcome at 7 to 12 days.
More adverse effects in treated group, number needed to harm (NNH) = 9.
Start antibiotics if no improvement by day 7 or patient has worsening at any time.
Amoxicillin should be first choice based on safety, efficacy, cost, and narrow spectrum. A 10-14 day course is commonly used (7 days beyond clinical improvement).
Treatment of Chronic Sinusitis
Saline lavage (Ann Fam Medicine, July 2006).
Intranasal steroids (INS)
Antihistamines – not useful, may worsen by drying mucosa. Only consider if significant allergic component.
Itraconazole (Sporanox) for fungal sinusitis (most commonly seen in the Southern states). Itraconazole use requires a close follow-up due to the risk of CHF, cardiac arrhythmias, liver dysfunction and peripheral neuropathy (foot drop). It has a "black box" warning for CHF patients.
Refer to ENT for chronic sinusitis. Balloon sinuplasty is a procedure gaining wider acceptance.
Nasal Polyps
Nasal polyps can be considered a form of chronic hyperplastic sinusitis and usually originate in the ethmoid sinuses. Malignant transformation is uncommon. Polyps can occupy the entire nasal cavity, thus producing a total blockage.
Nasal polyposis can be associated with allergic fungal sinusitis, cystic fibrosis (CF) and the triad of asthma, aspirin intolerance, and nasal polyps (Samter's triad in AERD). In cystic fibrosis, polyps show neutrophilic inflammation.
CF should always be considered in children with nasal polyps.
What is the triad of aspirin-exacerbated respiratory disease (AERD)?
Samter's triad include asthma, aspirin sensitivity, and nasal/ethmoidal polyposis:
ASPirin
Asthma
Sensitivity to aspirin
Polyps
Approximately 9% of the U.S. population has asthma - 9% of adult asthmatics have aspirin-exacerbated respiratory disease (AERD) (http://goo.gl/FIeE9).
Noneosinophilic sinusitis is considered to have an infectious basis and is treated with antibiotics. Organisms found are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. If a patient has Pseudomonas aeruginosa or Staphylococcus aureus, cystic fibrosis should be considered in differential diagnosis.
Diagnosis
A limited CT of sinuses costs about the same as a standard plain film sinus series but is much more useful.
CT scan findings do not correlate well with symptoms.
Upper airway endoscopy can identify anatomic or mechanical disorders of the upper airway. Anterior rhinoscopy is an examination of the nasal cavity performed with a nasal speculum under good illumination. Usually done with a rigid rhinoscope.
The gold standard for diagnosis of bacterial sinusitis is sinus puncture and culture.
Treatment
Treatment of Acute Sinusitis
Over 70% of patients with acute rhinosinusitis improve after 7 days, with or without antimicrobial therapy.
NNT = 7: 7 patients must be treated to achieve one additional positive outcome at 7 to 12 days.
More adverse effects in treated group, number needed to harm (NNH) = 9.
Start antibiotics if no improvement by day 7 or patient has worsening at any time.
Amoxicillin should be first choice based on safety, efficacy, cost, and narrow spectrum. A 10-14 day course is commonly used (7 days beyond clinical improvement).
Treatment of Chronic Sinusitis
Saline lavage (Ann Fam Medicine, July 2006).
Intranasal steroids (INS)
Antihistamines – not useful, may worsen by drying mucosa. Only consider if significant allergic component.
Itraconazole (Sporanox) for fungal sinusitis (most commonly seen in the Southern states). Itraconazole use requires a close follow-up due to the risk of CHF, cardiac arrhythmias, liver dysfunction and peripheral neuropathy (foot drop). It has a "black box" warning for CHF patients.
Refer to ENT for chronic sinusitis. Balloon sinuplasty is a procedure gaining wider acceptance.
Nasal Polyps
Nasal polyps can be considered a form of chronic hyperplastic sinusitis and usually originate in the ethmoid sinuses. Malignant transformation is uncommon. Polyps can occupy the entire nasal cavity, thus producing a total blockage.
Nasal polyposis can be associated with allergic fungal sinusitis, cystic fibrosis (CF) and the triad of asthma, aspirin intolerance, and nasal polyps (Samter's triad in AERD). In cystic fibrosis, polyps show neutrophilic inflammation.
CF should always be considered in children with nasal polyps.
What is the triad of aspirin-exacerbated respiratory disease (AERD)?
Samter's triad include asthma, aspirin sensitivity, and nasal/ethmoidal polyposis:
ASPirin
Asthma
Sensitivity to aspirin
Polyps
Approximately 9% of the U.S. population has asthma - 9% of adult asthmatics have aspirin-exacerbated respiratory disease (AERD) (http://goo.gl/FIeE9).
Pediatric sinusitis (click the link to continue).
Surgical treatment of chronic sinusitis
References
Allergy and Immunology MKSAP, 3rd edition.
Acute and Chronic Rhinosinusitis: Practical Clinical Treatment Strategies. Nancy Otto, PharmD. Medscape, 11/2008.
Acute Sinusitis: A Cost-Effective Approach to Diagnosis and Treatment. AFP, 1998.
Sinusitis Practice Guideline Aims to Improve Diagnosis, Cut Antibiotic Use. AFP, 2007.
Related Reading
FIT Corner Questions. Chapter 78 of the 6th edition of Middleton’s Allergy Principles and Practice, edited by N. Franklin Adkinson, et al. September 27, 2006. Chapter 78: Nasal Polyps and Sinusitis.
Allergic Fungal Sinusitis. Photoclinic. Consultant. Vol. 48 No. 9, August 1, 2008.
JAMA Patient Page: Acute Sinusitis, 2009.
Surgical treatment of chronic sinusitis
Functional Endoscopic Sinus Surgery (FESS) is the surgical standard of care. FESS restores sinus drainage and provides some symptom improvement in close to 90% of selected patients.
References
Allergy and Immunology MKSAP, 3rd edition.
Pediatric sinusitis. Ellen R. Wald, MD. Audio-Digest Pediatrics, Volume 55, Issue 14, July 21, 2009.
Acute Bacterial Rhinosinusitis in Adults: Part II. Treatment. AFP, 2004.Acute and Chronic Rhinosinusitis: Practical Clinical Treatment Strategies. Nancy Otto, PharmD. Medscape, 11/2008.
Acute Sinusitis: A Cost-Effective Approach to Diagnosis and Treatment. AFP, 1998.
Sinusitis Practice Guideline Aims to Improve Diagnosis, Cut Antibiotic Use. AFP, 2007.
Related Reading
FIT Corner Questions. Chapter 78 of the 6th edition of Middleton’s Allergy Principles and Practice, edited by N. Franklin Adkinson, et al. September 27, 2006. Chapter 78: Nasal Polyps and Sinusitis.
Allergic Fungal Sinusitis. Photoclinic. Consultant. Vol. 48 No. 9, August 1, 2008.
JAMA Patient Page: Acute Sinusitis, 2009.
Humming increases airflow between the sinus and nasal cavities, which could protect against sinus infections. NYTimes, 2010.
Multi-symptom Asthma is Closely Related to Nasal Blockage, Rhinorrhea and Symptoms of Chronic Rhinosinusitis http://goo.gl/sU4AU
Nucleotide-binding oligomerization domain (NOD)-like receptors (NLRs) have a potential role in chronic rhinosinusitis/polyps http://goo.gl/QAS4r
Atrophic Rhinosinusitis: Progress Toward Explanation of an Unsolved Medical Mystery. Medscape, 2011.
SNOT-16 Assessment Tool for Acute Sinusitis takes 5 minutes - copyright protected by Washington University. Medscape, 2011.
Staphylococcus aureus biofilm and and superantigens are associated with chronic sinusitis, cause T-helper 2 skewing http://bit.ly/ngnxBe
Intranasal antinuclear autoantibodies (ANA) in patients with chronic rhinosinusitis with nasal polyps. JACI, 2011.
Chronic Sinusitis - JAMA Patient Page (PDF), 2011.
Mnemonics for sinusitis: PODS and C-PODS (end of PDF here)
Published: 07/10/2007
Updated: 04/29/2012
SNOT-16 Assessment Tool for Acute Sinusitis takes 5 minutes - copyright protected by Washington University. Medscape, 2011.
Staphylococcus aureus biofilm and and superantigens are associated with chronic sinusitis, cause T-helper 2 skewing http://bit.ly/ngnxBe
Intranasal antinuclear autoantibodies (ANA) in patients with chronic rhinosinusitis with nasal polyps. JACI, 2011.
Chronic Sinusitis - JAMA Patient Page (PDF), 2011.
Mnemonics for sinusitis: PODS and C-PODS (end of PDF here)
Published: 07/10/2007
Updated: 04/29/2012
Subscribe to:
Posts (Atom)